Obesity is more than just a weight concern—it is a health condition linked with several chronic illnesses, most notably type 2 diabetes. Many people often ask, “Can Obesity Patients Have Diabetes?” This is an important question because excess weight does not only affect appearance but also impacts the body’s metabolism, blood sugar regulation, and overall health. Understanding the connection between obesity and diabetes can help individuals take proactive steps to prevent or manage these conditions.
The Strong Link Between Obesity and Diabetes
Medical research consistently shows that obesity is one of the strongest risk factors for developing type 2 diabetes. When excess fat accumulates in the body, especially around the abdomen, it interferes with insulin’s ability to regulate blood sugar. This causes insulin resistance, a state in which the body’s cells stop responding effectively to insulin. Over time, blood sugar levels rise, and type 2 diabetes develops.
The answer to the question “Can Obesity Patients Have Diabetes” is therefore yes—obesity significantly increases the chances of diabetes. However, it is important to remember that not every obese individual will develop diabetes, and not every person with diabetes is obese. Factors such as heredity, daily habits, and environment play a part as well.
Why Excess Weight Matters
Excess body fat triggers chronic low-grade inflammation, which disrupts normal metabolic functions. This inflammation causes changes in hormones, increases blood pressure, and worsens cholesterol levels—all of which raise the risk of diabetes.
Belly Fat and Insulin Resistance
Abdominal fat is particularly dangerous. Unlike fat stored in the hips or thighs, belly fat produces inflammatory chemicals that make insulin less effective. This is why people with central obesity (larger waist circumference) are at a higher risk of type 2 diabetes compared to those with fat distributed elsewhere.
Other Risk Factors to Consider
While obesity is a key contributor, additional factors like age, family history, poor diet, stress, and lack of exercise also influence diabetes risk. Combining these with obesity makes the likelihood of developing type 2 diabetes much higher.
Can Obesity Patients Have Diabetes? Signs to Watch Out For
Early signs of diabetes can be subtle. Being overweight often makes these symptoms more pronounced. Watch for:
- Constant thirst and frequent urination
- Unexplained weight changes
- Fatigue and low energy
- Blurred vision
- Slow-healing wounds
If these symptoms appear, it’s wise to consult a doctor for proper screening.
Preventing and Managing Diabetes in Obese Individuals
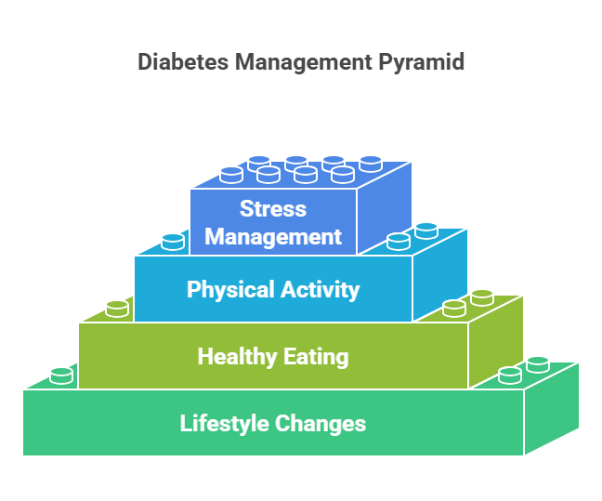
The good news is that lifestyle changes can greatly reduce the risk of diabetes, even for people who are obese. In fact, studies show that losing just 5–10% of body weight can significantly improve insulin sensitivity and lower blood sugar levels.
Healthy Eating
Choosing a diet rich in vegetables, lean proteins, whole grains, and healthy fats can make a big difference. Avoiding sugary drinks, processed foods, and refined carbs is also crucial for weight and blood sugar control.
Physical Activity
Regular workouts improve the body’s efficiency in handling insulin. A mix of aerobic workouts, such as walking or cycling, combined with strength training provides the best benefits. Just 30 minutes of daily physical activity can help reduce diabetes risk.
Stress and Sleep Management
Chronic stress and lack of sleep raise cortisol levels, which increase hunger and cravings, making weight loss more difficult. Practicing relaxation techniques, maintaining a bedtime routine, and reducing screen time can help improve both sleep and stress levels.
Obesity and Diabetes – The Path Forward
So, can obesity patients have diabetes? Obesity stands as one of the primary contributors to type 2 diabetes. While not every obese person will develop diabetes, the chances are significantly higher compared to those with a healthy weight. The encouraging news is that lifestyle changes, medical guidance, and regular health check-ups can prevent, delay, or effectively manage diabetes in obese individuals.
Taking small but consistent steps—such as improving diet, staying active, reducing stress, and maintaining a healthy sleep schedule—can protect long-term health and reduce the risk of complications. Ultimately, prevention is always better than treatment, and the journey toward better health starts with informed choices today.
At Erode Diabetes Foundation (EDF), in collaboration with MMCH, we focus on early action to prevent and manage diabetes. Obesity is a key risk factor, but with lifestyle changes and medical support, your health can improve. Our Body Composition Analyser (BCA) helps to assess obesity levels in detail and plan personalized therapy. We provide consultations, nutritional guidance, and diabetes-focused care for long-term wellness. Remember, even simple steps a healthy meal, a short walk, or a check-up can make a big difference.


